By David Shultz | Nov. 26, 2014 , 2:00 PM
Humans have been using antibody therapies to treat infectious disease for more than 100 years. Blood plasma from influenza survivors administered to sick patients in 1912 may have contributed to their dramatic turnaround. In the years since, immune proteins from survivors have been administered to infected individuals in an attempt to combat diseases like Lassa fever, SARS, and even Ebola.
It’s hard, however, to find survivors who can donate plasma containing these lifesaving immune proteins. Now, a team led by researchers at the U.S. Army Medical Research Institute of Infectious Diseases (USAMRIID) in Frederick, Maryland, has used genetically engineered cows to produce large amounts of human antibodies against hantavirus, an often deadly disease mainly transmitted from rodents to people. In animal models, at least, these antibodies provided robust protection against the virus, opening the door to therapies to treat and prevent hantavirus, for which there is no cure. The bioproduction technique also holds promise for generating antibodies against other infectious agents.
The work is preliminary and needs to be tested in people, but the team calls it a “proof-of-concept” that human antibodies can be grown in animals and retain their activity against disease.
“I’m personally very excited about it. I think that this offers potential for treatment of patients with hantavirus infection,” says Greg Mertz, an infectious disease specialist at the University of New Mexico, Albuquerque, who was not involved in the research. “If you extrapolate this to other diseases, there are some where this approach might be promising.”
The USAMRIID researchers, led by virologist Jay Hooper, teamed up with SAB Biotherapeutics in Sioux Falls, South Dakota, to use genetically engineered cows that, when presented with an antigen, could produce fully human polyclonal antibodies against both the Sin Nombre hantavirus strain, first isolated from the Four Corners region of the southwestern United Sates, and the Andes hantavirus strain, which is prevalent in Chile. There, it infects an average of 55 people annually and kills about a third of them. After a lengthy incubation period and a few days of fever and muscle aches, the virus attacks the lungs and often causes acute respiratory failure leading to death. There is no cure, and the experimental vaccines would be logistically challenging to use even if they passed clinical trials.
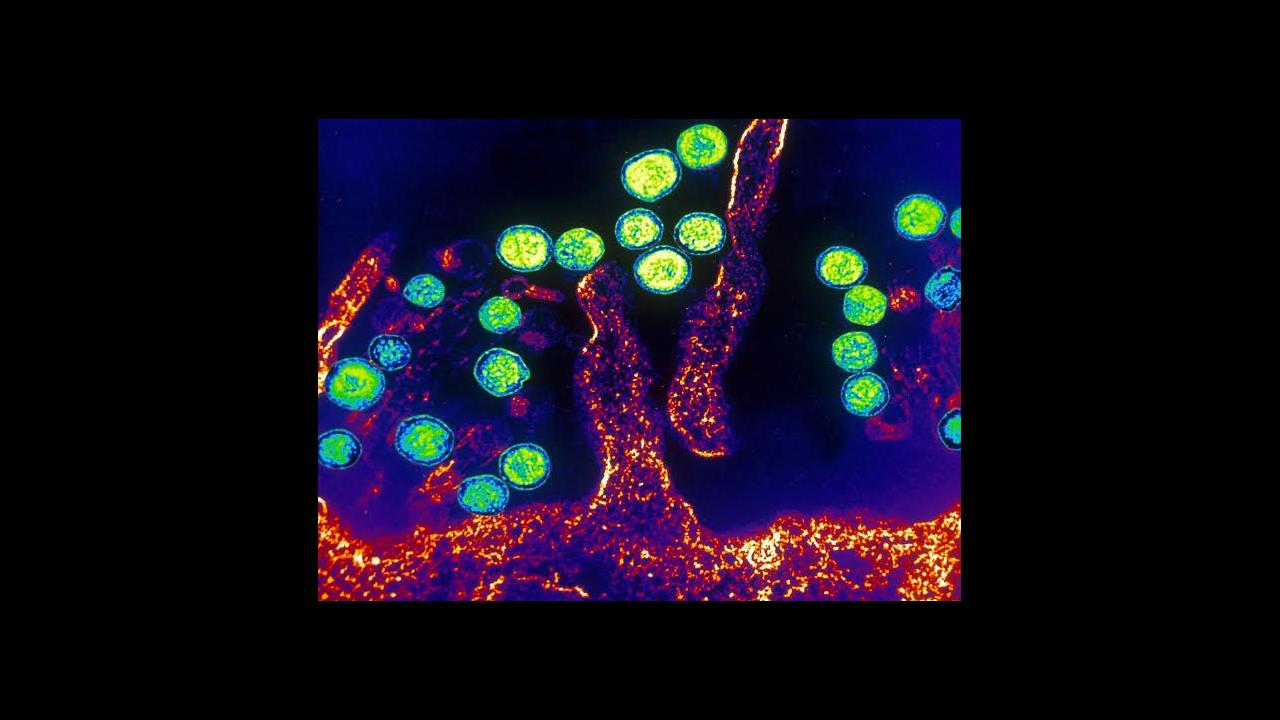
Creating human antibodies in an animal model is no small feat. Scientists combined parts of human chromosome 14 and human chromosome 2—the bits that are needed to produce antibodies—into an artificial chromosome and implanted it in cows. The genes responsible for producing cow antibodies were silenced. As a result, the bovines produced immune cells that spit out human antibodies.
Scientists then administered experimental hantavirus DNA vaccines, against the Andes and Sin Nombre strains, to the “transchromosomal” cows. Within a month, the animals were producing liters of high-concentration human antibodies against both strains. The scientists then extracted the immune proteins and used them to treat hamsters that had been lethally infected with hantavirus. The treatment increased the hamsters’ chances of survival dramatically, saving seven out of eight infected with the Chilean hantavirus strain, while all eight controls died, the team reports online today in Science Translational Medicine. Five of the eight hamsters infected with the Sin Nombre strain were rescued.
Animal models don’t always translate to humans, but in this case the research team is optimistic. Nonhuman antibodies from, for instance, birds and primates, have been safely administered to people in the past, so human antibodies are expected to prove safe in phase 1 clinical trials, says reproductive physiologist Eddie Sullivan of SAB Biotherapeutics, who headed the project to develop the transchromosomal cows. Nor does he suspect that the antibodies would cease to function in humans. If anything, they may work better because they’ll be able to communicate with human immune cells more fluently, he says. “We expect that the antibodies will likely be very well tolerated in humans and will respond similarly,” Sullivan says.
Of course, nothing is certain. In very rare instances, some previous antibody therapies have actually helped viruses reproduce in cells by serving as a bridge to host cells. “In order to really finish the proof-of-concept, clinical studies in humans showing safety need to be performed,” Hooper says. “If this material turns out to be as easy to produce as it seems, and it’s safe, I think it’s a great, great way to move forward.”
The USAMRIID scientists are also investigating cutting out the bovine middleman and simply giving their hantavirus vaccines straight to people. But antibody therapies are actually more practical in some respects. In diseases like hantavirus, where so few people are infected every year, a large-scale vaccination program might not make much sense, especially from an economic standpoint, Hooper says. Having a few doses of antibodies on hand to treat the unlucky few infected people could solve the problem without the need to vaccinate huge swaths of the population. Furthermore, Sullivan notes, a single cow can produce antibodies against multiple strains of the virus in copious amounts, up to 1000 human doses per month.
A huge challenge for any potential treatment for hantaviruses is finding a way to diagnose the disease in time. The infection is difficult to recognize before it moves to the lungs, at which point it’s often too late. Having an available supply of hantavirus antibodies on hand could allow health workers to administer treatment to people who’ve come in contact with an index case, Mertz says.
Again, the potential benefits still hinge on clinical trials that show safety and efficacy; the team is optimistic they could begin as early as next year for hantavirus, and maybe even sooner for other diseases. “We’re working on Ebola and also MERS-CoV,” Sullivan says.
https://www.sciencemag.org/news/2014/11/cows-human-chromosomes-enlisted-fight-hantavirus